Healthy North Coast is one of 5 Primary Health Networks (PHNs) participating in the DiRECT-Australia study, with 5 general practices from the Ballina/Byron, Clarence Valley, Coffs Harbour and Richmond Valley regions involved in the project.
Diabetes Australia NSW & ACT have released this media release.
New research could revolutionise the way type 2 diabetes is treated in Australia, potentially helping millions of Australians, now and in the future, avoid diabetes complications and severe illness.
The DiRECT-Australia study, being undertaken by Diabetes NSW & ACT, five Primary Health Networks (PHNs), and the University of Sydney, is trialling whether a structured weight management and lifestyle program can trigger remission of type 2 diabetes.
With more than 1.2 million Australians diagnosed with the condition and a further 500,000 who have developed type 2 diabetes but are not yet aware of it, the results of this study could change the quality of life for patients and save the health system billions of dollars.
Watch the 7NEWS report on the DiRECT-Aus study:
The research is replicating the UK DiRECT study in Australia to determine if the remission results can be achieved here.
In the UK study’s results, published in the Lancet:
- 46% of participants in the intervention group achieved type 2 diabetes remission.
- Of those in remission after one year, 70% stayed in remission.
- Remission is closely linked to weight loss: two-thirds of those who lost 10 kilos or more and 86% of those who lost 15 kilos or more achieved remission.
- ·Weight management program also resulted in better quality of life and reduced need for diabetes medications compared to standard care.
One of the research leads, endocrinologist Tania Markovic, is a clinical associate professor at the Boden Collaboration and Sydney Medical School, University of Sydney, and Senior Staff Specialist in the Department of Endocrinology, Royal Prince Alfred Hospital, Sydney.
Assoc Prof Markovic says the UK research debunks the belief that type 2 is an inevitably progressive condition.
“The results from the UK indicate that type 2 diabetes can be halted and people can achieve remission after diagnosis,” Assoc Prof Markovic said.
“It’s important that we understand we’re talking about remission, not a cure. If people regain weight, type 2 will resume. This study has the potential to give diabetes patients different outcomes than we’ve achieved with traditional treatments, such as medications, in the past.”
As well as resulting in remission for many participants, the UK program led to fewer diabetes medications across the whole intervention group.
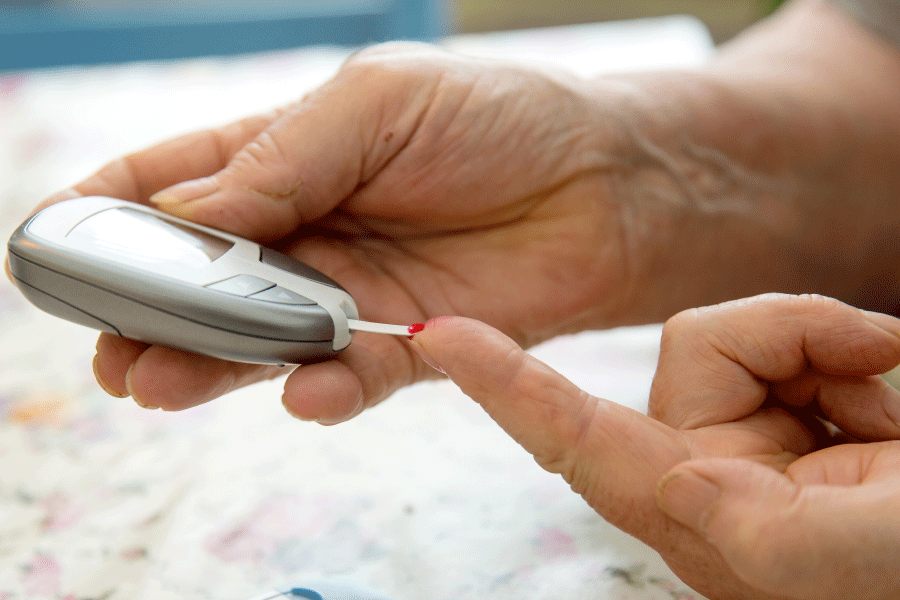
Remission of type 2 diabetes means blood glucose levels are in the normal range without diabetes medication. In clinical terms, this means an HbA1c (a blood test that shows your average glucose levels over two to three months) of 6.5% or 48 mmol/mol, or lower, while not taking diabetes medications for at least the previous two months.
Assoc Prof Markovic said complications from diabetes include heart and kidney disease, stroke, blindness, amputations, and depression.
Diabetes NSW & ACT’s DiRECT-Aus Project Lead, Kate Gudorf, said research participants receive meal replacement shakes and bars, education and regular appointments with a dietitian.
“The dietitian helps people move through the diet phases, starting with meal replacements and later moving to a healthy, calorie-controlled diet,” Kate said.
“It’s not easy to lose weight and keep it off so we offer support throughout the program, including individual and group meetings with a dietitian.
“The meetings cover a range of topics to help participants make lifestyle changes, such as improving food choices and increasing physical activity. These meetings are designed to support people to change behaviour and maintain weight loss.”
Sydney North Health Network Primary Care Advancement General Manager, Deb Pallavicini, said the PHNs’ investment in the DiRECT research could help people with type 2 diabetes slow or prevent long-term complications.
It could also save the Australian health system billions of dollars by avoiding acute intervention and hospitalisations in the long term.
“As a result of the DiRECT study in the UK, type 2 diabetes remission programs are now becoming widely available there,” Ms Pallavicini said.
“Sydney North PHN has become involved in this research as we think Australia could achieve similar outcomes to the UK, which would allow this intervention to be widely used in Australia, too.”
Visit Primary Care Impact for more information about the project:
DiRECT-Aus Diabetes Remission Replication Project
Visit HealthPathways for localised information on diabetes.
Username: manchealth
Password: conn3ct3d