Menu
May
15
2018

Dr Adrian Gilliland is a Coffs Harbour general practitioner, chair of NCPHN’s Mid North Coast (MNC) Clinical Council and board member of the MNC Division of General Practice. He has been a key GP involved in the development of the Safe Transition of Care Program on the NSW North Coast.
Dr Gilliland spoke with the joint LHD/PHN Project Manager, Isabel Butron, regarding regional NSW impacts on patients and providers.
Isabel: Dr Gilliland, patients outside of the urban centres often have to wait longer or travel more to see a GP or access emergency care. And when they do, they often assume their care-related information flows seamlessly back to their GP or hospital doctors. From your experience, what sorts of challenges surround care transfers and are there any specific issues in regional/rural settings?
Dr Gilliland: Busy GPs, ED doctors and health professionals often need to share electronic summaries that community-based GPs and nurses need to pick up and continue. In rural and remote Australia, where there are limited services and greater workforce pressures, it is even more important that GPs get timely messages regarding what happened to their patient in hospital or in ED and vice versa.
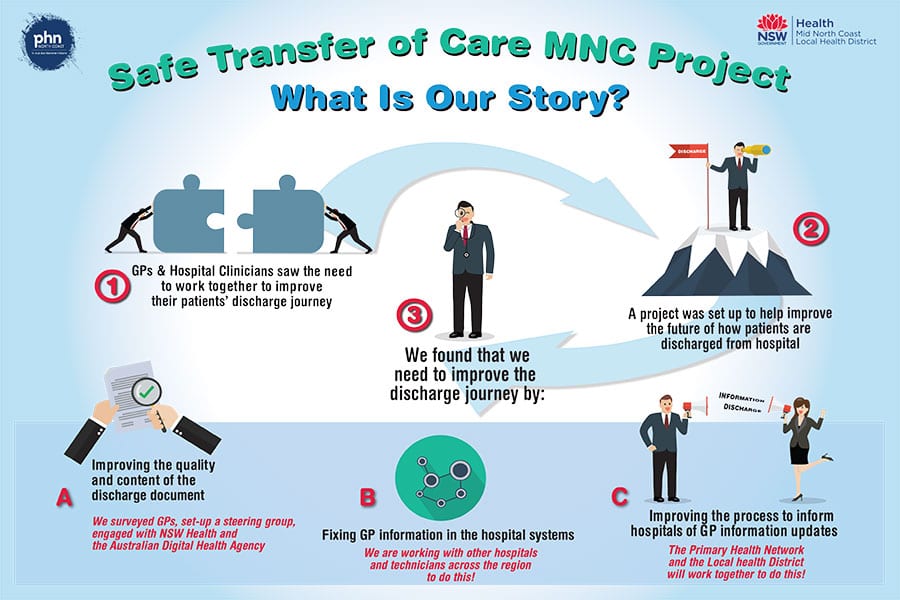
In this project we’ve seen many examples where transfer or discharge summaries were sent but not received, and where hospitals see the same patients return due to missed opportunities in the community. Both sectors often struggle to fix these issues alone. Not receiving the discharge summaries adds further time spent running around to get the information while we should be using this time focusing on our patient’s needs. Some of our patients need to travel a substantial distance to see us – the idea of not knowing that the patient has been in hospital is a very serious concern.
Isabel: So how did the project get clinical input regarding these challenges around shared electronic communications, and what kinds of areas did it focus on?
Dr Gilliland: Clinicians raised the issues and concerns in a number of forums. We heard that the timeliness and quality of the discharge summaries were inconsistent across the board. As a network group we just didn’t know how to go about trying to rectify the problem and what the actual barriers were. Therefore, in collaboration with the PHN and our local LHDs, we sought to identify these barriers and provide recommendations for improving the timeliness and quality of discharge summaries. We also did a survey that received unheard of response rates and we spoke with a range of leaders locally, regionally and in other settings, eg. eHealth.
Isabel: The Rural Health Alliance is a key body that can provide leadership in developing and prioritising critical communication enablers such as this. Given this project was designed to investigate and recommend broader more complex reforms, what are the key messages that rural and regional leaders can advocate on or influence wherever possible?
Dr Gilliland: We are still finalising our recommendations in partnership with NSW Ministry/eHealth, the MNCLHD and NCPHN, but it seems clear that the timeliness and quality of this kind of information is extremely critical for the safety and high standard of care our rural and regional patients and health professionals deserve. RHA is a strong advocate for getting high-quality medical services in place in regional and remote areas, however the actual work supporting these professionals to communicate effectively once established is sometimes overlooked. This is a vital message that RHA could advocate for.
Isabel: Dr Gilliland, as stated above, you have been instrumental in advocacy and support of this program across the North Coast. What do you think has been unique in this project and have you seen benefits from this project in your own practice?
Dr Gilliland: This project has undeniably had some big impacts to the North Coast. We have seen a stronger relationship formed between each of the hospitals and the PHN with hospitals. The relationship we now have across the major stakeholders has seen shared planning and shared solutions contribute to a better outcome.
The benefit realised to date within my own practice is that we have seen an increase in the timeliness of discharge summaries coming in. We now have a concise discharge notification from our Emergency Department. We have seen an increase in the receipt of Mental Health discharge summaries. Overall we are confident that we will see an increase of the timeliness of discharge summaries and an improvement in the quality.
Isabel: Finally Dr Gilliland, what is the message or statement you would like to say to our regional area?
Dr Gilliland: The Safe Transition of Care is a big piece of work and we have only begun. We are yet to implement further solutions and recommendations across with our LHD partners. Looking at the future we will need to focus on Primary Care changes and improvements.
We want to continuously improve to ensure our patient’s safety.
A word from Dr Grant Rogers, Rural eMeds Chief Medical Officer/Clinical Lead, Rural eHealth Program:
“With the coming of eMeds implementation to 112 sites across the six rural LHDs, we hope this will contribute to the quality of discharge summaries and enhance the Transition of Care efforts to date. Integrating care between LHDs, PHNs and primary care (GPs and Community Health) services is vital in improving the patient’s journey. Every effort is being made to improve the flow of clinical information across the healthcare spectrum.”
Flu Vaccination Program Now Mandatory
The Maze of Medicinal Cannabis