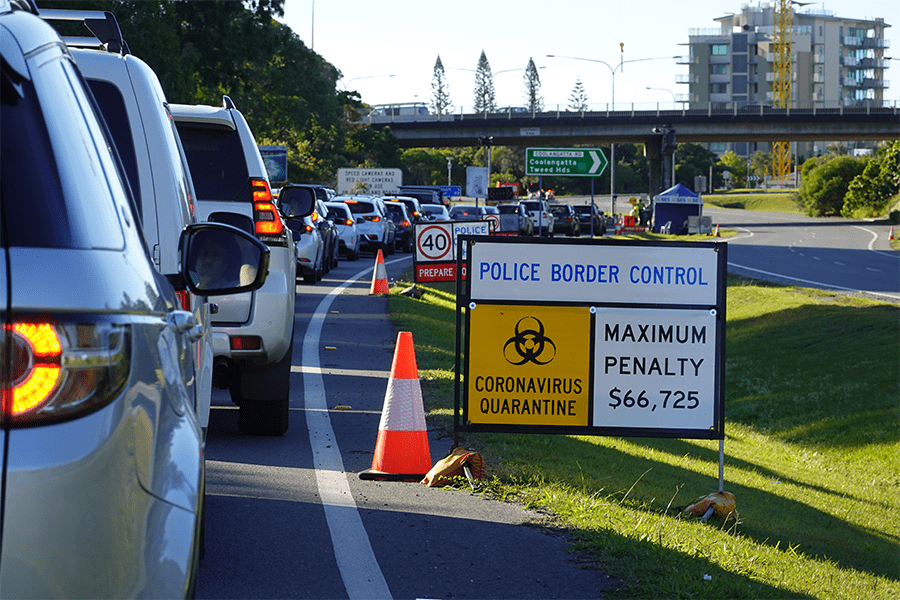
The Northern NSW health workforce and community are understandably concerned about the implications of the Queensland border restrictions.
Healthy North Coast is working closely with the Northern NSW Local Health District to advocate for the needs of our practitioner community. We are in contact with Queensland Health, the Gold Coast Public Health Unit and Gold Coast PHN, and will provide you with updated information as this becomes available.
Healthy North Coast will continue to contact local clinicians and service providers to understand the impact these changes are having, so that together we can anticipate appropriate response measures and action where and when required.
Northern NSW Patients Update
Queensland Health has provided updated guidance for Northern NSW residents outside the border zone who need to access specialist medical care in Queensland.
NSW residents living outside the border zone can continue to enter Queensland to obtain specialist health care that is not available in their place of residence. Eligible residents must apply for a Queensland Border Declaration Pass (General). Click here to learn more.
Patients will need to present a copy of their border pass as well as a letter from their specialist with the day/time of their appointment at the border crossing.
Patients attending a day treatment or appointment will not be required to quarantine but must leave Queensland immediately following their appointment.
Further details regarding the definition of specialist health care and the requirements for quarantine for different patient groups and carers are available in this media release from NSW Health.
Telehealth
We encourage all practitioners to make use of telehealth at this time. The list of telehealth MBS items has continued to expand since first announced in March 2020 and incorporates general practice, mental health, allied health and nursing services. The current list of items is available here.
Specialist services may also be available via telehealth. MBS items are available for general practitioners to support patients to access specialist services via telehealth. We encourage practitioners to explore this option with your patients. The healthdirect Video Call service is available free of charge to clinicians and Healthy North Coast can assist practitioners to register for this service. Please get in touch if you would like to find out more.
Healthy North Coast also commissions a range of mental health telehealth services through the Connect to Wellbeing program. These services are all available by telephone or video. GPs providing mental health care to patients can also access specialist advice and case management support via the GP Psychiatry Support Line.
Business Continuity Planning
Healthy North Coast is working closely with the Local Health District and other partners to identify strategies to support our acute and primary care workforce. We are also advocating to our local Members of Parliament and relevant ministers to promote patient-centred decision making that both manages risk and prioritises access to essential health services.
In the interest of preparedness, we encourage practices to explore options for business continuity planning in the event that further restrictions eventuate. Telehealth will form a major part of this planning, and we are also exploring strategies to mitigate staff impacts.
We understand that the border restrictions are causing anxiety for practitioners and community members. A continued focus on physical distancing, good hygiene, and encouraging early testing is our best defence against COVID-19.
Border Closure Impact Feedback
Help us support you! We want to hear from practices who are impacted by the border closure or may be impacted if the restrictions are further tightened. Understanding the scale of the impact will help us to better target our advocacy and support.
We would also like to hear from health professionals who have not been impacted, and who may have capacity to help out neighbouring practices that are experiencing staff shortages.
Photo by Igor Corovic / Shutterstock.com